PhD Studentship via the GW4 BioMed2 MRC Doctoral Training Programme
Rationale
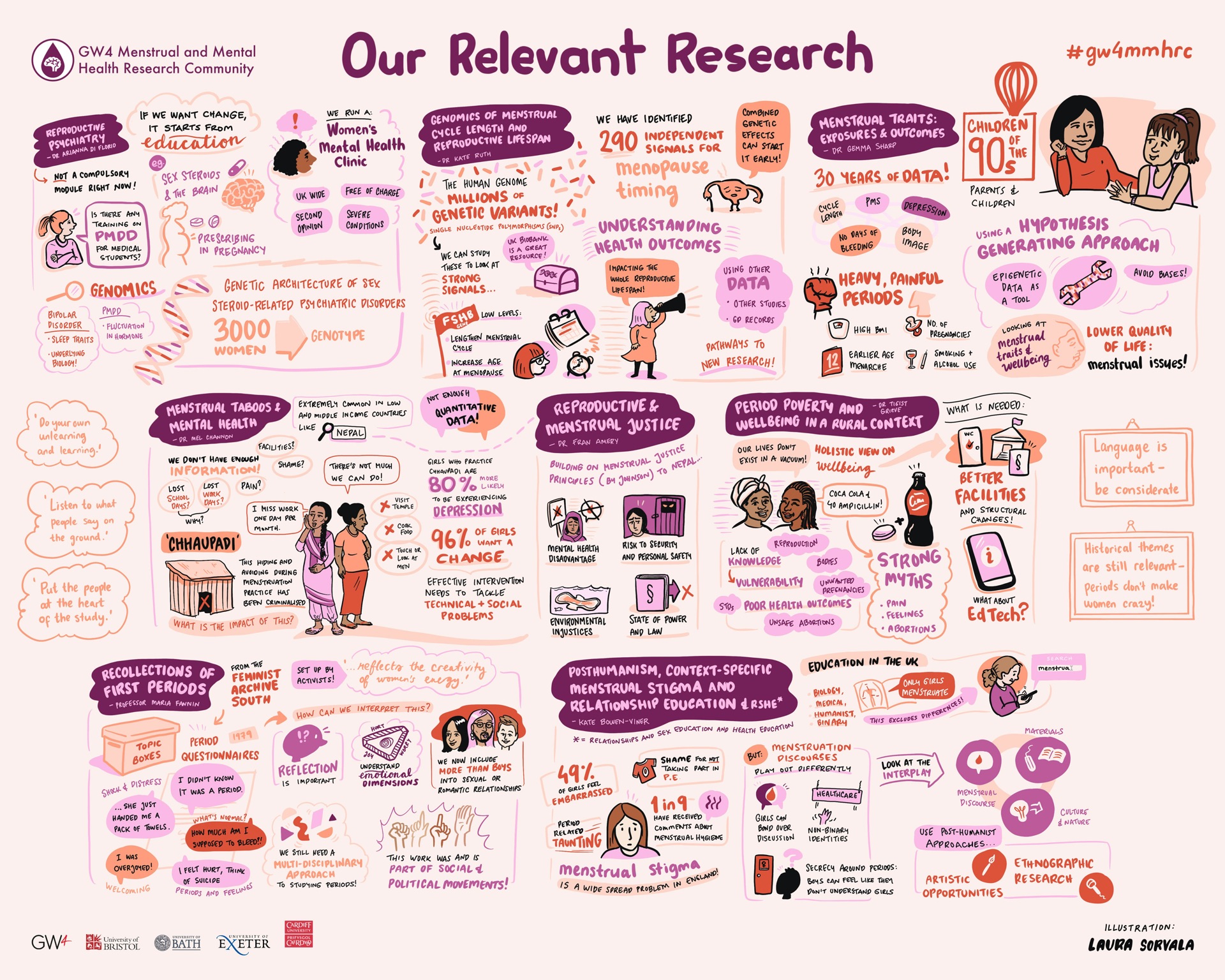
Problematic menstrual symptoms such as heavy menstrual bleeding (HMB) are common and distressing, impacting substantially on quality of life and mental wellbeing of affected women. As well as this likely effect of HMB on poor mental health (MH), there could also be an effect in the reverse direction: psychological stress is also a known disruptor of menstrual cycles and can be associated with heavier bleeding. Additionally, HMB is almost always self-reported and measured subjectively (with reduced quality of life now being part of the official diagnosis), so an association between HMB and MH might be explained by women with mood disorders being more likely to assess their level of bleeding as abnormal and substantially affecting their quality of life.
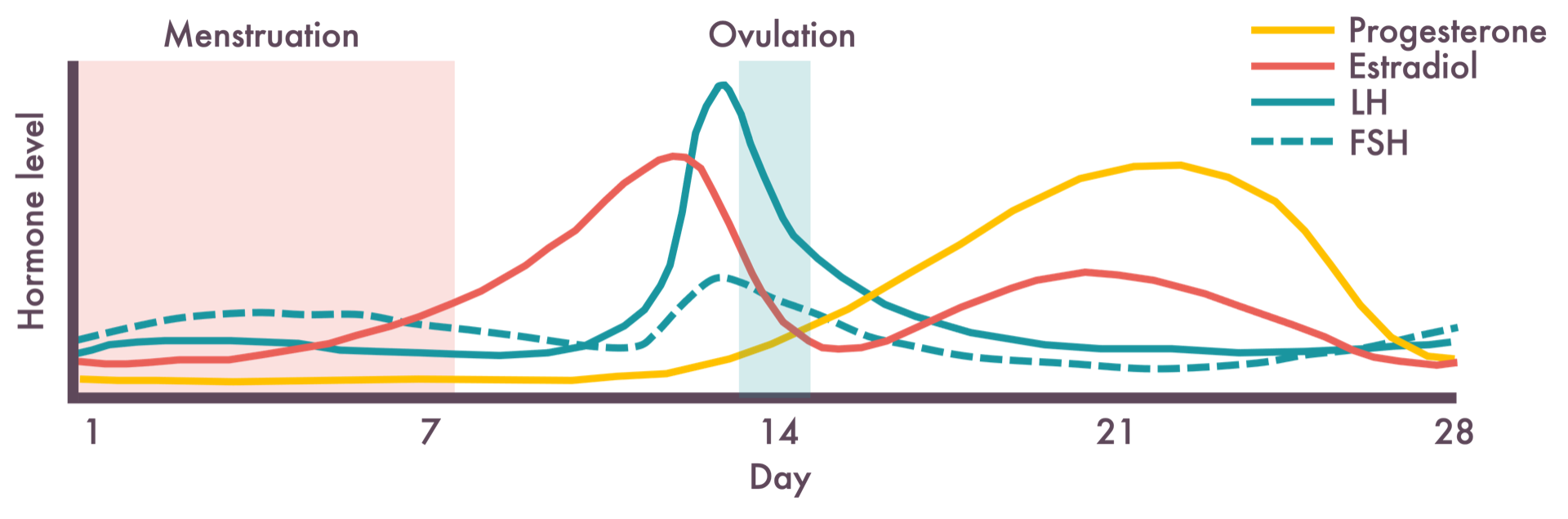
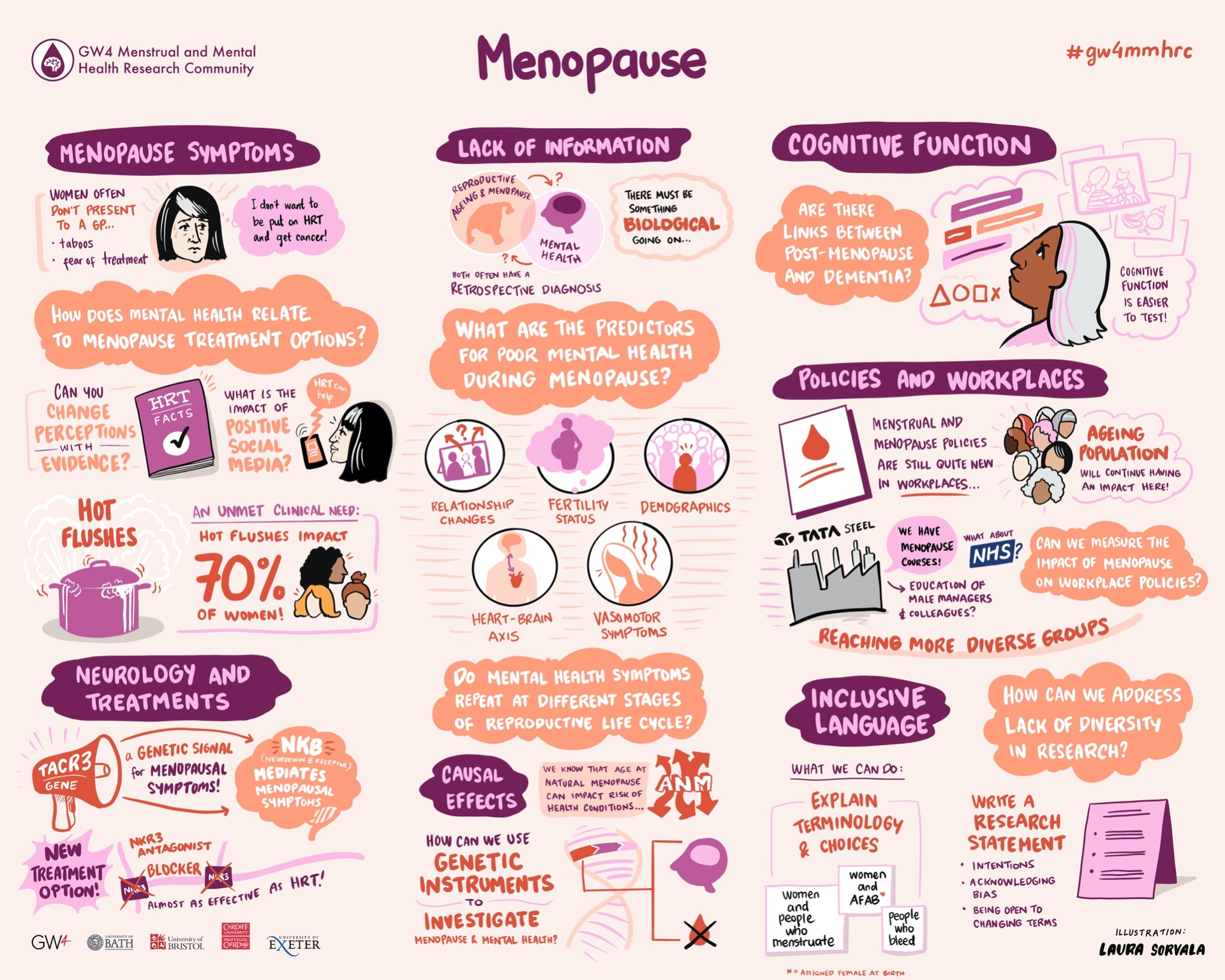
Both HMB and MH are influenced by inflammation. Increasing evidence suggests that inflammation plays a causal role in the pathogenesis of psychiatric disorders, including depression, and inflammation is also known to show cyclical variation, partly influenced by fluctuations in reproductive hormones throughout the menstrual cycle. There is also some evidence that systemic and local endometrial inflammation is associated with severity of menstrual symptoms like HMB.
Aims & Objectives
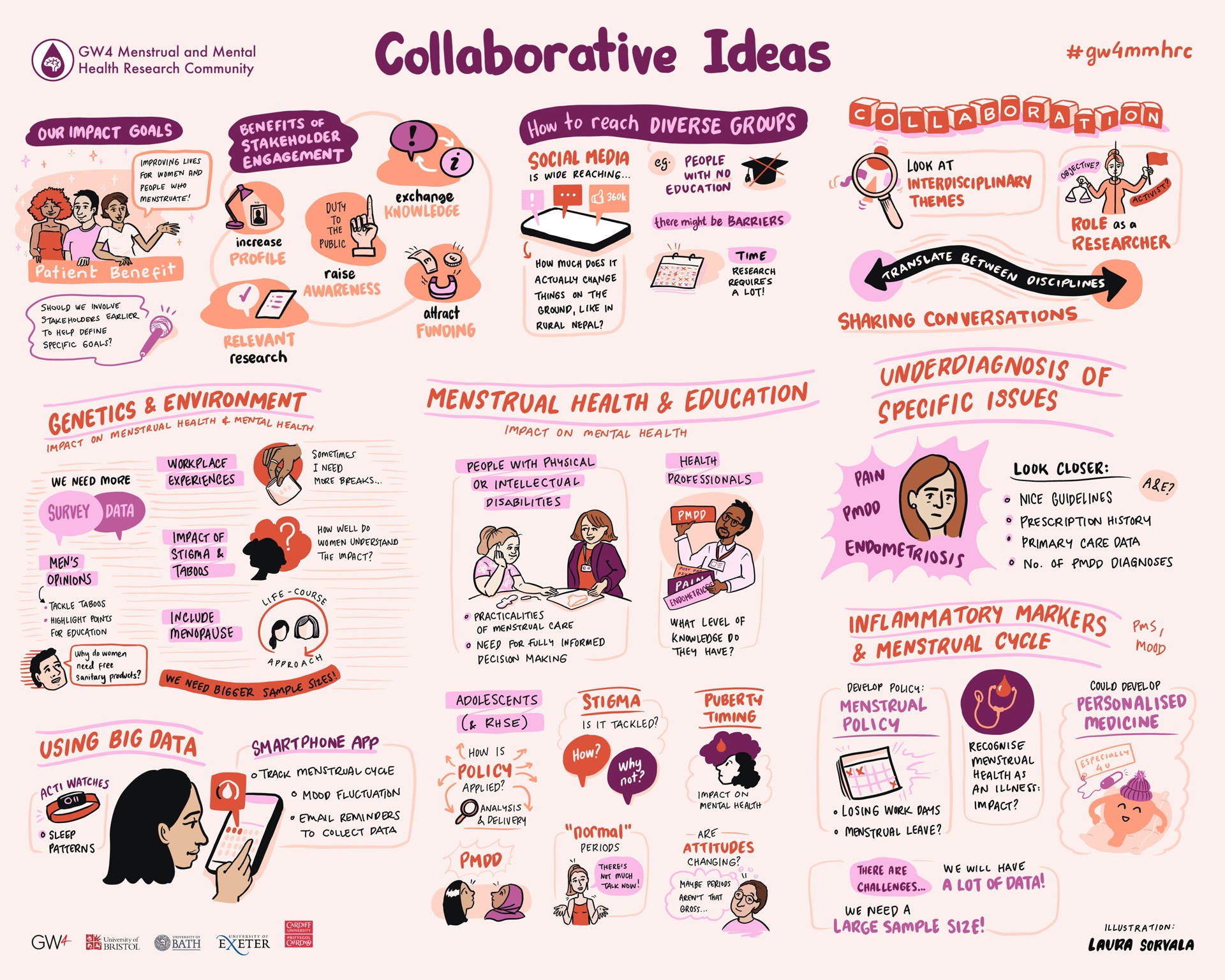
This project aims to explore direct effects of HMB on MH, and of MH on HMB, as well as the potential confounding or mediating role of inflammation. A better understanding of these relationships would help inform ways to predict whether women with HMB are at greater risk of MH conditions, and whether women with MH conditions are at greater risk of menstrual issues like HMB. This would help clinicians tailor care to improve outcomes for groups of women. Understanding whether these associations are likely to be causal, and whether inflammation plays a role in the manifestation of both HMB and MH conditions will help shed light on the pathogenesis of HMB (and underlying pathologies) and MH and suggest whether both could be effectively treated using anti-inflammatory medications.
Methods
This project will use a genetic epidemiology approach to examine bi-directional associations between HMB and MH, as well as the role of inflammation in explaining any relationship. The student will first examine the association between HMB and MH phenotypes in UK Biobank and the Avon Longitudinal Study of Parents and Children (ALSPAC). Then, using results from our previous genome-wide association study (GWAS) of HMB in UK Biobank, the student will generate polygenic risk scores (PRS) for HMB in UK Biobank and ALSPAC and conduct reduced-phenome-wide association studies (PheWAS) to identify MH variables and inflammatory biomarkers associated with genetic liability to HMB. The student will also use LD score regression (LDSR) to explore the genetic correlation between all traits of interest using our HMB GWAS results and results from previously published GWAS of MH conditions and inflammatory biomarkers. Any associations from the pheWAS and LDSR will be followed up using Mendelian Randomization (MR) to explore if relationships are likely to be causal.
The student will learn to apply 2 MR approaches: 1) 1-sample MR (this will allow us to test MR assumptions using individual-level data), 2) 2-sample MR using GWAS summary statistics (this will improve power above the one sample MR).
Sensitivity analyses will allow the student to explore assumptions of both methods.
The student will also explore effects in the opposite direction by using results of previous GWAS of MH conditions and inflammatory biomarkers to generate PRS in ALSPAC and UK Biobank and test for associations with HMB, as well as in 1 and 2 sample MR analyses to explore causality.
The student will triangulate findings from across the PRS and MR analyses to inform network MR analysis including HMB, MH and inflammation to explore the strength and direction of direct and indirect and combined and independent causal effects.
How to apply
Student applications can be made via the GW4 BioMed2 website: https://www.gw4biomed.ac.uk. The closing date for applications is 5pm on Friday, 26th November 2021. Shortlisted applicants will be invited for an informal interview (over the phone, on Skype or Zoom) between Monday 31st January 2022 and Friday 11th February 2022. The formal interviews will be held virtually on the 16th and 17th February 2022.
A GW4 BioMed2 MRC DTP studentship includes full tuition fees at the UK/Home rate, a stipend at the minimum UKRI rate (£15,609 for 21/22), a Research & Training Support Grant (RTSG) valued between £2,000-£5,000 per year and £300 annual travel and conference grant based on a 3.5-year full-time studentship. These funding arrangements will be adjusted pro-rata for part-time studentships.
The GW4 BioMed2 MRC DTP studentships are available to UK, EU and International applicants. The GW4 institutions have all agreed to cover the difference in cost between home and international tuition fees. This means that International candidates will not be expected to cover this cost.
For any informal queries about the studentship, please contact Gemma Sharp (gemma.sharp@bristol.ac.uk).